OBESITY AND METABOLIC SURGERY
This surgical intervention is aimed at patients suffering from severe obesity or from a metabolic syndrome such as type 2 diabetes.
It is carried out in conjunction with interprofessional teams and the attending physician. This treatment is part of a personalised pathway for the patient.
It is strictly regulated by the French High Authority for Health (HAS).
A bespoke preoperative care programme is designed for each patient in order to minimize surgical complications and to optimize the outcome in the medium and long term.
These pages will guide you through the different stages of this care, and provide the information to help you better understand the management of your obesity.
presentation of the Hepato Digestive Unit team

Prof. Didier MUTTER
Head of unit

Dr. Michel VIX
Head of the Bariatric and Metabolic Surgery Programme

Prof. Silvana PERRETTA
Head of the Bariatric and Metabolic Endoscopy Programme

Dr. Mihaela IGNAT
General and digestive surgery

Dr. Déborah KADOCHE
General and digestive surgery

Dr. Michele DIANA
General and digestive surgery
What is obesity?
Obesity is excess weight due to an increase in body fat. It has been recognised as a disease since 1997 by the WHO. Its prevention and treatment is a public health issue.
Obesity is defined by a Body Mass Index (BMI) greater than 30. Above 40, obesity is said to be severe or morbid.
BODY MASS INDEX (BMI) CALCULATOR
You can calculate your BMI on www.calculersonimc.fr
Severe obesity is a real health risk. It causes or contributes to:
- non-insulin-dependent diabetes (also called type 2 diabetes)
- sleep apnea
- high blood pressure
- several types of cancer (colon, breast, uterus, etc.)
It is often associated with a metabolic syndrome.
Causes
In industrialised countries, obesity is the consequence of unhealthy eating habits combined with an inadequate lifestyle. We are indeed witnessing a craze for fast food (ready meals, fast food…) often unbalanced because it is too high in fat and energy in a small amount of food.
Comfort eating, in the form of snacking, is often a response to a stress-inducing lifestyle. The predominance of intellectual work or forced inactivity (unemployment), excessive use of the car, long hours spent in front of screens, are all factors that promote sedentary lifestyles and therefore obesity.
In France, over 30% of the population is overweight and 12% of adults are obese, with an increase in severe obesity cases. This latter form of obesity disrupts social and professional life, but above all is detrimental to physical health and wellbeing.
metabolic syndrome
This term refers to the association of a number of health problems due to poor body metabolism.
Its definition evolves and is refined over time, and combines at least 3 of the following factors:
- Abdominal” obesity: waist circumference greater than 100 cm for men and 88 cm for women
- High blood pressure
- A decrease in cholesterol – HDL or “good cholesterol”)
- An increase in triglycerides
- Carbohydrate metabolism disorders, ranging from hyperglycemia to type 2 diabetes
The causes are common to obesity, although genetics may play a role. A sedentary lifestyle and a diet high in calories (sugars and fat) are the main factors.
does it apply to me?
Obesity surgery is regulated in France by the French High Autority for Health (HAS).
Obesity surgery can be considered if you have a BMI (see BMI calculator) greater than 40, or greater than 35 with a complication of obesity (for example: hypertension, diabetes, osteoarthritis, sleep apnea).
There are some contraindications:
- Age: under 18 or over 65 years old
- Serious and/or progressive diseases: infectious (AIDS, viral hepatitis), cancer, inflammatory bowel disease (Crohn’s disease, rectocolitis, etc.)
- Untreated mental health disorders
- Severe addictions to alcohol or drugs
The HAS recommendations date from 2009 and are still current
bespoke programme
The surgical management of obesity is based on 4 aspects in order to enable and maintain a good outcome for the patient:
- dietary management before and after surgery
- mental health assessment and follow-up before and after surgery
- the surgery itself
- regular and sustained physical activity according to physical possibilities
Surgery alone will only provide an average and short-lived outcome if other measures are neglected.
The patient is therefore offered a multifaceted pre-operative pathway. After having set up the dietary, psychological and behavioral care, a pre-surgery check-up is carried out.
This is intended to minimise the medical risks of the surgical procedure and to check for possible contraindications to certain surgical techniques.
Your attending physician is a key player in this care and is in contact with the surgical team, the endocrinologist and the mental health professional.
This pre-operative care process takes place over 6 months at least.
Providing information for patients is very important, and many documents are available, including those of the HAS.
Example: “Obesity Surgery: What you need to know before you decide“
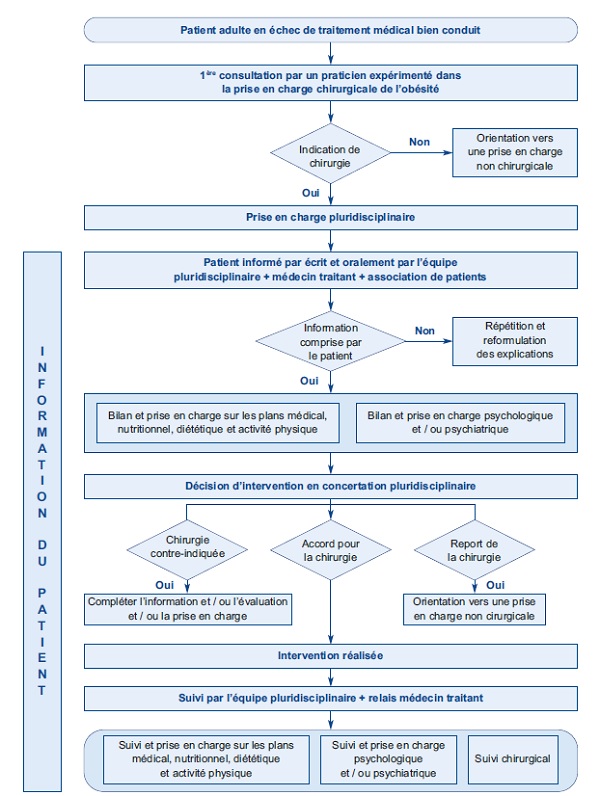
pre-operative care pathway
Step 1
- Nutritional and mental health follow-up,
- Dental consultation to check for the absence of oral foci and to assess chewing capacity,
- Search for sleep apnea by a neurologist, pneumologist or endocrinologist. The discovery of this disorder will require the use of an appliance at night and does not contraindicate surgery,
- Performing a gastroscopy to look for an esophageal or gastric abnormality: gastroesophageal reflux or hiatus hernia will be a contraindication to a sleeve gastrectomy. A gastric biopsy will be carried out to verify the absence of Helicobacter pylori infection (if present, a treatment will eradicate it).
Step 2
Pre-operative check-up in day hospital.
This stage takes place over one day and includes:
- A cardiological evaluation including an ECG and a cardiac ultrasound. This is to check the absence of an unknown cardiovascular pathology or to reassess a cardiovascular disorder already dealt with,
- An anesthesia consultation to explain the anesthetic aspects of the procedure and the pain management protocol,
- An abdominal ultrasound to look for biliary lithiasis and assess the extent of liver steatosis,
- An x-ray of the oesophagus and stomach to check for hiatal hernia,
- A dietary consultation explaining the good dietary rules in post-operative period with the presentation of the renutrition plan,
- A physiotherapy consultation to prepare for the operation and post-operative remobilization,
- A surgery consultation to answer questions concerning the preoperative assessment and the planning of the procedure.
Step 3
The last consultation is to provide a case summary and to discuss with the patient the most appropriate intervention for their case and request.
The patient signs a personal “commitment“.
The surgeon establishes the surgical indication, presents the file to a multidisciplinary committee and draws up the documents for health insurance coverage.
This multidisciplinary committee (RCP – Réunion de Concertation Multidisciplinaire) is mandatory in France.
The surgeon files a PAD – Request for Pre-Surgery Agreement.
A date for the surgery is set.
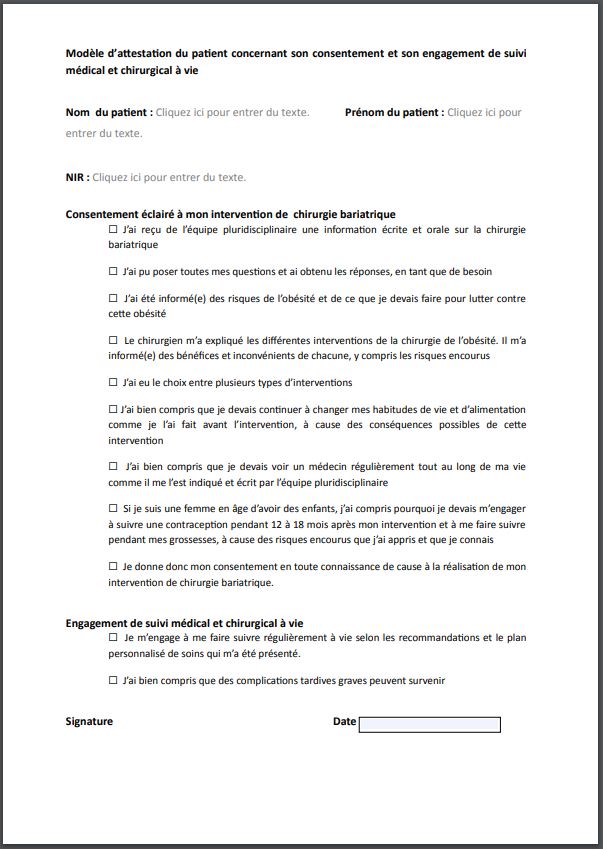
Personal undertaking / template of patient certificate attached to the request for prior agreement
![]() See the consent template in .pdf format (*Only in French version)
See the consent template in .pdf format (*Only in French version)
the surgical timeline
2 weeks before
You are asked to follow a low-fat, high-protein diet designed mainly to reduce liver volume and intra-abdominal fat.
1 week before
You will be asked to have a preoperative blood test and to have the result with you when you are hospitalized.
Hospitalization
You will be hospitalized the day before (or the day of) the operation. The nursing team will welcome you and explain the practical aspects of your preparation for the operation.
Your surgeon will visit you in the late afternoon to answer your questions.
On the day of the operation
Surgery start times are estimates only, as some procedures can take longer than expected depending on anatomy and issues relating to the patient.
The different procedures available require general anaesthesia.
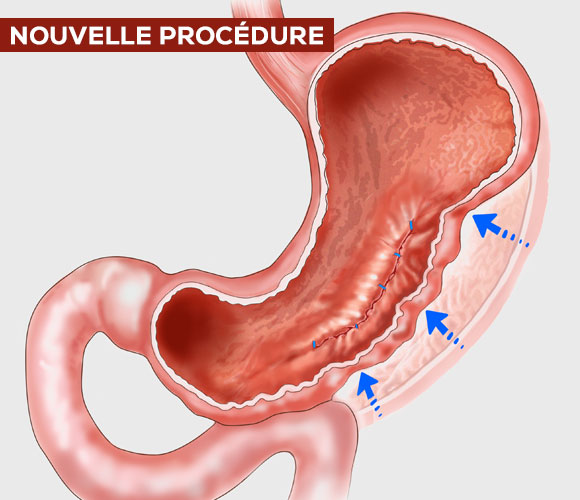
The operation is performed by laparoscopy or endoscopy (Endosleeve).
The duration of the operation varies according to the operating technique chosen.
Pain medication will be given to you intravenously.
The surgical team will be able to call a contact from your family or friends after the surgery.
Therefore, make sure that you have designated this person and that you have communicated their telephone number.
When you wake up
After the procedure, you will stay in the recovery room for about two hours before returning to your room.
You will be able to drink water or herbal tea that evening.
The nursing team will assist you in standing up for the first time.
The vein access will be removed that same evening or the following day.
A liquid diet will then be started.
The dietician will explain the food intake program and its evolution for the next few weeks.
You will leave between the 1st and 3rd post-operative day and you will be seen again for the removal of the stitches 8 days following surgery.
In many cases, ambulatory care with a specific follow-up is offered.
post-operative follow-up
First control at 8 days
Checking for scars. Removing the sutures.
Assessment of pain and dietary follow-up.
Consultation at 1 month
Assessment of pain and dietary follow-up.
Prescription of hygieno-dietary rules.
Consultation at 3 months
Weight monitoring.
Evaluation of physical activity and dietary follow-up.
Consultation at 6 and 12 months
Weight monitoring.
Evaluation of physical and dietary possibilities.
Annual control
Weight monitoring.
Verification of the absence of deficiencies and if necessary supplementation.
From 6 months
It will be necessary to resume a follow-up by the nutritional endocrinologist.
Psychological follow-up may also be useful to facilitate adoption of the diet and body shape.
Since 2018, an “endoscopic” follow-up is recommended:
Endoscopic monitoring after Sleeve Gastrectomy and Gastric Bypass in omega :
=> Recommended: Gastroscopy at 1 year and 3 years
=> Mandatory: Gastroscopy at 5 and 10 years post-surgery
In case of EBO (Endobrachyoesophagus) :
=> Contraindication (relative) to the gastrectomy Sleeve.
=> Monitoring every 2 to 5 years
=> Discuss converting a Sleeve to Gastric ByPass
Ref : Obésité (2018), Vol13, N°4:207-208.
post-operative eating
During your stay, a dietician will provide you with a programme to resume eating regular foods. This document details the steps for gradually restoring the eating function.
In general
Normal eating is difficult immediately after the procedure.
The absorption of water is easy but in small sips only.
We advise you to start by drinking using a spoon.

The pureed diet is not very appetizing but enables good healing of the suture lines in the stomach or small intestine.

Red meat, pasta and rice are poorly tolerated during the first few months, even if they are well chewed.

If you notice a reduction in food possibilities and/or very frequent vomiting (several times a week or several times a day), you should consult your surgeon who will look for the reasons for this dysphagia, and give you vitamins intravenously.
Intravenous vitamin supplementation is now routinely recommended in cases of major eating disorders, vomiting, dysphagia and in any emergency situation.
complications
Complications may occur after the procedure as with any type of surgery. They affect 3% of patients. The aim of the exhaustive pre-operative check-up is to reduce the risk of complications.
Complications can be of a general nature. We will mention the main ones, without being exhaustive: a pulmonary embolism (gas or venous) may occur during or after the operation. Infections, which can be detected early or late after several weeks, and haemorrhages can occur.
Complications may be more specific and directly related to the procedure performed.
The following can be observed:
- A leakage at the anastomosis
This is manifested by abdominal pain, fever, a decrease in the volume of urine, tachycardia. The patient is then asked to return to the hospital to be diagnosed and treated in the department where the operation was performed. It may be necessary to intervene surgically, by radiological and/or endoscopic means, to treat these complications. The care may last several weeks. - Haemorrhage occurring during or at the end of the operation may require appropriate therapy, by surgery, endoscopy or interventional radiology
- An infection in the abdominal incisions
The thickness of the adipose tissue which is not well vascularized makes the healing of the abdominal incisions more difficult, and an abscess may appear on these incisions. Drainage is carried out to allow healing of this localized condition. - Herniation at the surgical incisions
Despite the care taken to close the surgical incisions, the rapid weight loss after the operation weakens the parietal sutures and may result in the appearance of a hernia. Surgical repair may be necessary and will be performed by our medical team. - Eating disorders, discomfort when swallowing
The surgical intervention modifies the digestive circuit and requires adaptation of the diet. This is explained during the pre-operative care and in the post-operative care before the patient is discharged. However, dietary habits are difficult to change. Most of the time, another explanation of the instructions is sufficient to enable a correct diet. In some rarer cases, a narrowing of the anastomoses between the different organs is noted. This may require dilatation by endoscopy. - Vitamin disorders
The reduction of the diet and the change in the digestive system requires regular vitamin level monitoring A vitamin complex is systematically prescribed as soon as the patient is discharged. It should also be noted that there can be vitamin disorders before surgery, related to an unbalanced diet. It is therefore essential to follow the consultation plan established by the surgeon and the endocrinologist to enable the (easy) correction of these vitamin disorders.
SURGICAL TECHNIQUES
The choice of the surgical procedure is determined at the end of the preoperative assessment. This one allows to detect the possible contraindications for certain types of interventions. It is primordial to be aware of the advantages and risks of complications that may occur in the short or long term.
We are with your listening, your opinion is taken in consideration with the results of the preoperative assessment.
There are several possible surgical techniques depending on your personal situation.
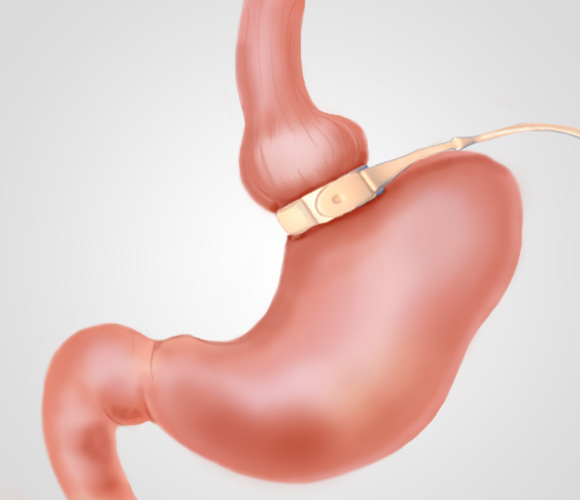
GASTRIC BANDING
ENDOSCOPIC GASTROPLASTY OR ENDOSLEEVE
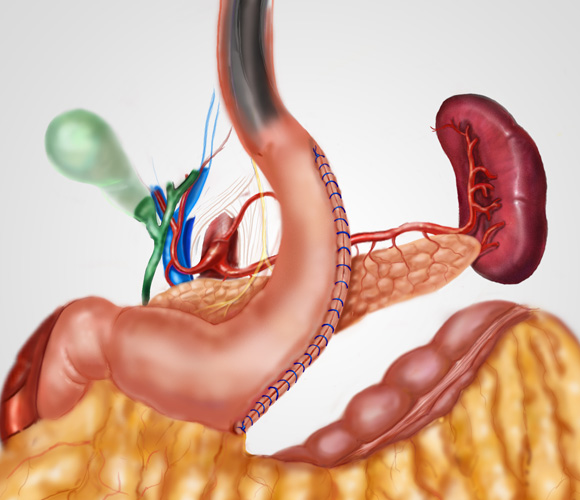
SLEEVE OR LONGITUDINAL GASTRECTOMY
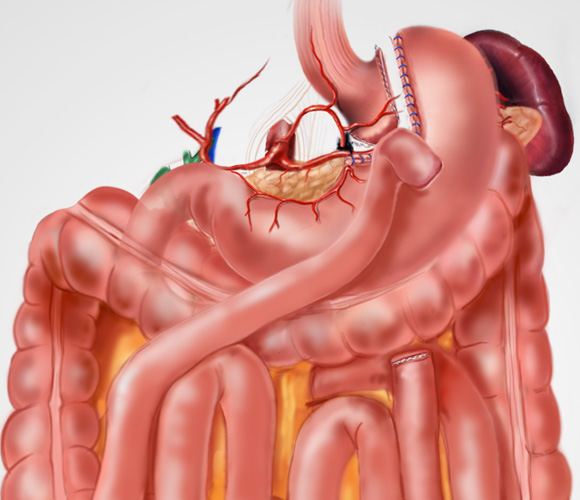
GASTRIC BYPASS
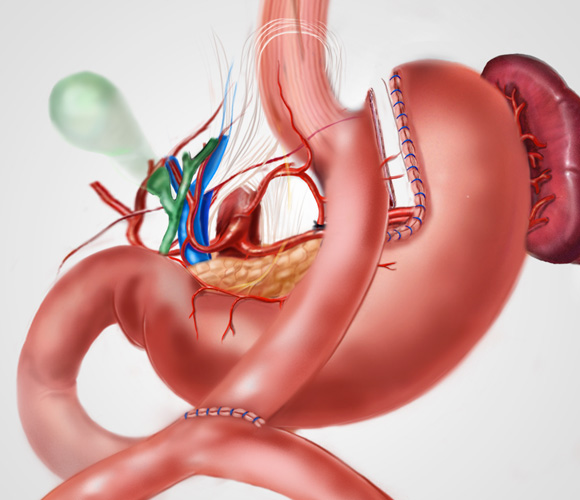
MINI GASTRIC BYPASS
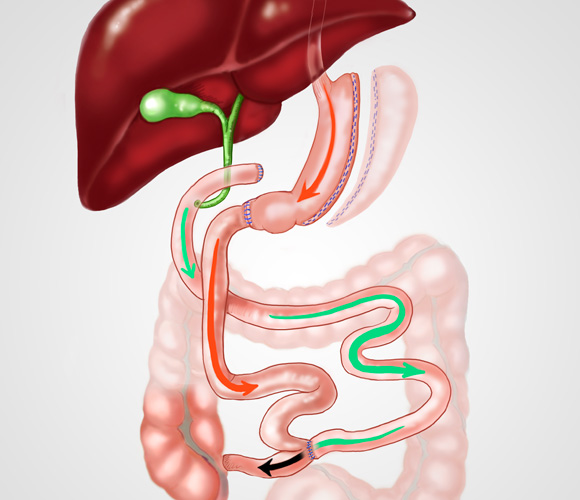
BILIO PANCREATIC BYPASS